By Dr Amenze Eguavoen
If you were to ask any young person in Nigeria today what their plans are, professionally or otherwise, they would outline the steps they are taking to “japa” without missing a beat.

The exodus of Nigerians is not limited to young professionals, though; it is happening across all cadres. Nigeria is bleeding out its workforce at an alarming rate, and by default, we are providing skilled workers at a highly subsidized rate to economies that are willing to pay the right price in terms of salaries, welfare packages, and societal packages.
While migrating Nigerians will miss the social capital they gained in Nigeria—a culture that is rapidly dwindling anyway—many will gladly trade it for a chance at life. One only has to ask how much of this social capital would be needed to survive and thrive in a country riddled with insecurity, poverty, and hunger thereby earning the term “the trenches” by Nigerians online.
Although most highly skilled sectors are experiencing a loss of professionals, the health sector has been badly hit.
This trend has existed for years, but the COVID-19 pandemic brought on a major push/pull dance where human resources for health (HRH) or healthcare workers experienced a greater pull from the Western world.
This pull presented in the form of deliberately simplified migration policies and processes, better pay, better work environments, functional and equipped hospitals, security, and access to basic amenities. Unfortunately, while the Western world pulled healthcare workers, Nigeria pushed through unpaid salaries, rising insecurity, soaring inflation rates, absence of personal protective equipment in hospitals, and a fragile healthcare system which left healthcare workers vulnerable to COVID-19 infection.
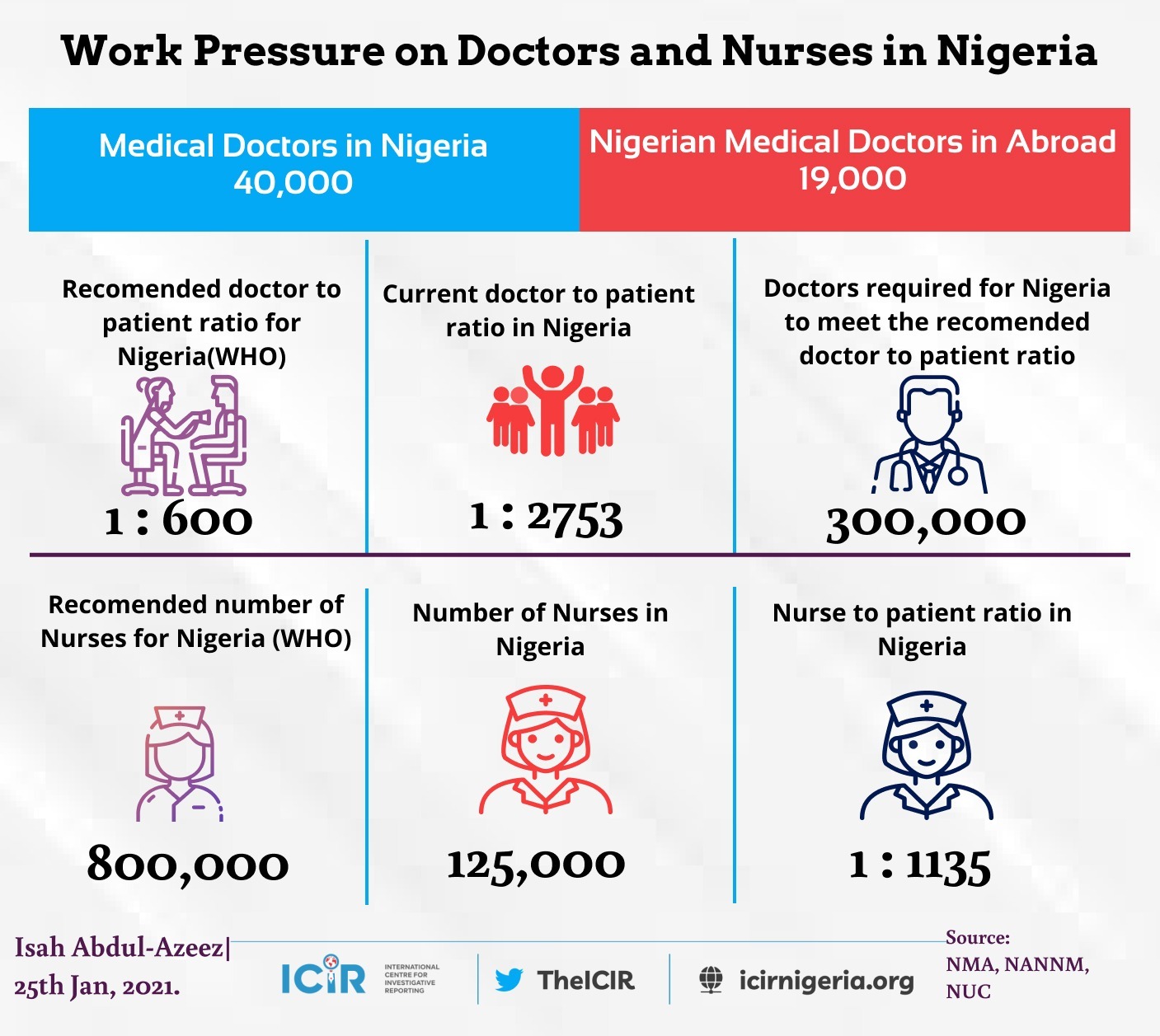
To improve health outcomes in Nigeria, such as life expectancy, maternal mortality, infant mortality, etc , the right quantity and mix of human capital resources are needed in the healthcare sector.
Presently, the country lacks a clear picture of its health workforce, although some states are working to address this.
Kaduna state, for instance, has a good sense of its health workforce profile and is using this information to plan.
Many states remain without an idea of how their health workforce is distributed.
There is an immediate need to conduct a mapping of the current health workforce in Nigeria to determine the number, spread, and type of health workers available, by gender, age, city type, years in service, etc. This will make it possible to identify the healthcare workforce needs that are in line with our health and disease profile.
It is not enough to say that a certain number of doctors or nurses are needed according to our population and WHO recommendations. Having that information is one part of the solution, more important, is knowing the skills and specialties needed by geographical location.
The rapid loss of healthcare workers has not been met with equal rate of employment; rather, the government has maintained an embargo on hiring in state and national institutions. To navigate the embargo, many healthcare facilities and state governments hire healthcare workers as volunteers contributing to the high rates of underemployment and poor job security which further underscores the willingness to migrate.

Assuming healthcare workers were being hired to meet the needs of the population, it would take Nigeria several years to meet the recommended healthcare workers to population ratio. Nigeria currently produces about 3,000 doctors and 14,000 nurses each year.
In Abia state alone, the Nigerian Medical Association reported that at least 2 doctors resign each month.
The limited capacity of various training institutions has contributed to the cap on number of healthcare workers produced annually. Many institutions are underfunded and have outdated facilities; while those that have some additional funding are not accredited to take on as many students as would be sufficient to fill the gaps. When these professionals are trained and employed, it would still take years to gain the experience that is required to function optimally and provide the quality of healthcare that is needed now!
For the active healthcare workers in the system, there is a glaring absence of a clear structure and path for capacity building that can be tracked and evaluated. This is particularly true for those who are outside of residency or formal training programs.
In other climes, certain trainings must be completed each year by health workers in various cadres of the health system. This training is specific to their current roles, and the renewal of their licenses is dependent on training completion thus ensuring a skill match necessary for provision of quality healthcare services.
In Nigeria, Continuous Medical Education is required for practicing licenses to be renewed, however, there are no specific course recommendations and courses taken are not tracked. A structured and predictable capacity building and career advancement plan will contribute to transparency, a clear sense of purpose and fulfilment for healthcare workers, which would potentially translate to increased productivity and retention.
If the government is serious about stemming the brain drain and ensuring the availability of healthcare workers in Nigeria, an intentional and multisectoral approach is vital for success. One that involves participation from stakeholders in different sectors and organizations such as: health, education, labour, and financial sectors; professional bodies, academic institutions, accreditation bodies, and civil society organizations.
The government needs to coordinate a stakeholders’ forum whose aim would be to dissect the issues and chart a clear and sustainable path for addressing them. Once that is done, the political will and resources to implement must be made available. The government should also be open and committed to developing policies that will make it easier to move resources, technology, and expertise from developed to developing nations.
All things considered, I dare say that political will is the major ingredient needed for any real positive change to be seen in the present situation with our human resources for health.







This iis very fascinating, You’re an excessively professional blogger.
I have joined your feed aand look ahead tto iin quewt off mlre of your wonderful post.
Also, I’ve share your site in myy social networks